What Getting 105 Blood Tests From a Health Startup Taught Me
Is it the future of health care—or too much data?


The last time I went to the doctor, I lived in a different zip code, belonged to a different body-weight category, and was rounding out a different decade. I never consciously swore off health care, but who likes feeling dismissed—or consistently being told that the next available appointment is months down the road?
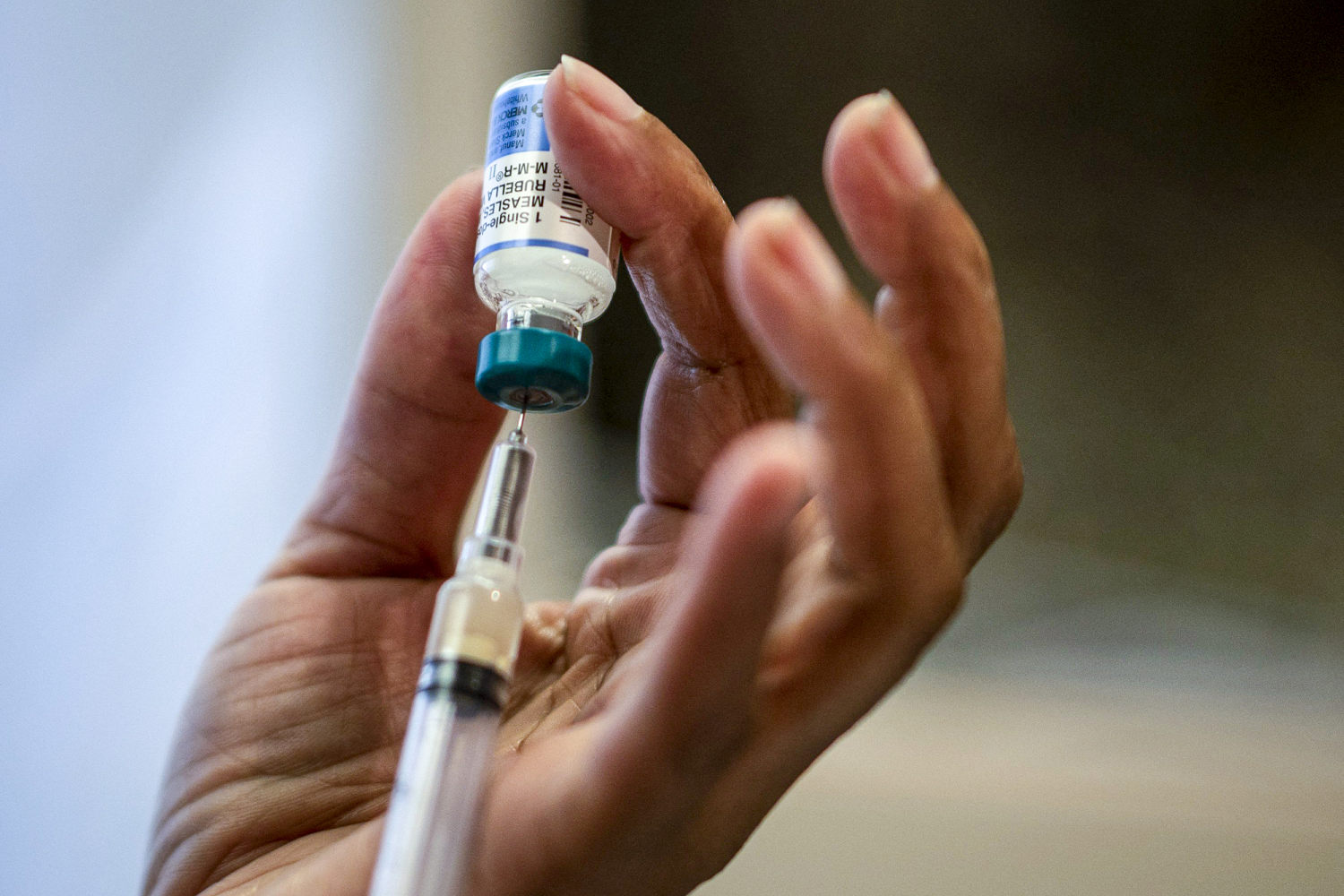
Yet after years of not stepping foot in an exam room, I knew I needed a check-up—make that a tune-up. That’s how I ended up in a phlebotomist’s chair at Quest Diagnostics at 7 a.m. on a recent Saturday, looking hard in the other direction to avoid seeing what felt like an excessive amount of blood pumping out of my arm. I had just joined Function Health, a personalized health testing platform co-founded by the preventive medicine guru Dr. Mark Hyman, and those dozen tiny vials would provide me with in-depth intel on more than 100 measures. I would soon receive a full assessment of my heart, hormones, thyroid, immunity, and seemingly every other aspect of my health. Was I nervous? Absolutely. Impatient for the results? You know it. [time-brightcove not-tgx=”true”]
Function Health—which launched in 2023 and bills itself as the fastest-growing health platform in the U.S.—is backed by big-name investors like Matt Damon, Zac Efron, Pedro Pascal, Jay Shetty, and Blake Griffin. The company is still in beta mode, which means you have to sign up for its waitlist; I was accepted within a day. For $499 per year, you get two rounds of testing: an initial assessment with 105 lab tests, and then three to six months later, a follow-up including 60-plus retests to see how your numbers are changing. By then, the Function team believes, you’ll have had the opportunity to make changes through diet, exercise, or a new medication regimen, and you’ll be able to see how those efforts are paying off. The hope is that people will remain members for years, tracking how their health evolves through twice-annual testing, and making changes that could add more quality years to their lives. While no treatment regimen is provided based on results, clients receive personalized written insights from Function’s team of clinicians.
For someone like me, who ignored annual-physical reminders and waited out even the most annoying symptoms, it seemed like an ideal way to get a much-needed health status update. But is putting patients in the driver’s seat of their own well-being the future of health care—or a slippery slope to information overload?
A pivot to proactive care
Hyman, 65, has spent his entire career trying to find a way to “break through the noise and really address chronic disease, which is now a national emergency,” he told me during a video conversation in September. He specializes in functional medicine, which aims to identify and treat the root cause of illness—not just the symptoms it triggers. In addition to being Function’s senior medical advisor, he’s the founder and senior advisor of the Cleveland Clinic Center for Functional Medicine, founder and director of The UltraWellness Center in Lenox, Mass., the author of a pile of books, and the host of a popular podcast. He regularly dispenses health tips to his 3 million Instagram followers: which inflammatory oils he avoids; how to think about brain-health supplements; what to know about the six states of insulin resistance.
He calls Function Health his most fulfilling venture. Hyman sees the startup as a natural extension of his desire to make medicine more proactive, pointing to a philosophy called P4 medicine, which stands for predictive, preventive, personalized, and participatory. The idea is to help people take control of their health by identifying what areas they need to work on before they land in a full-blown medical crisis. “The only way to do that is to have your own data, and not be limited by what you get at your doctor’s,” he says. “How do we break down the sort of patriarchal, paternalistic medical system that puts you apart from your own body? You have to go to the doctor and the insurance companies and ask for what you want, and they’re trained in a certain way which is essentially reactive, not proactive.”
Read More: When Should I Go to the Doctor With Cold Symptoms?
Function Health’s tests go beyond what many primary care doctors include in “outdated” annual panels, he adds. While doctors traditionally check LDL, HDL, and total cholesterol, for example, they don’t always include measures like lipoprotein(a), apolipoprotein B, and LDL pattern, all of which can predict future heart health. And while it’s common to find out your calcium and vitamin D levels, I’d never before had a doctor check my ferritin or iron binding capacity.
The thinking is that the earlier you realize something isn’t quite right, the sooner you can address it. Plus, Function’s platform is easy to navigate and visually pleasing—a welcome change from the poorly designed patient portals I was used to. That enables clients to track trends over time and compare their results from one round of testing to the next. Is their hemoglobin A1C gradually creeping up? Is their LDL cholesterol better or worse than it was six months or two years ago? Is that random kidney number still out of range, or was it a one-off blip?
“We’re very good at naming and blaming diseases,” Hyman says. “We’re not very good at identifying proactively, what is the transition from wellness to illness? Most people are just walking around with low, smoldering risk factors that they don’t know about.” He paused, meeting my eyes through the screen: “Like you, actually.”

My unexpected results
My first round of testing required nearly two dozen vials of blood, which could wipe you out for the day—so Function splits it into two separate appointments scheduled a week apart. On my second visit, the phlebotomist noticed I was starting to look pale and assured me fewer vials would be taken than the first time. When I left, fainting risk averted, she admitted she had lied. Still, by the time my results started rolling in a few days later, I had forgotten all about my sore arm. They arrived over the course of a week, during which I refreshed my Function Health portal constantly. Each time a measure was off, I dramatically declared that I was dying, and then proceeded to Google every possible explanation, working myself into a stupor.
During our interview, Hyman and I talked through my test results, which calmed my anxiety. (This one-on-one time isn’t customary for Function’s members, who typically receive insights without any one clinician’s name attached.) In total, 20 of my biomarkers were out of range, and 85 were normal. I learned, for example, that my thyroglobulin antibodies (TgAb) were above range—“low-grade Hashimoto’s,” Hyman speculated after reviewing my results—and that I had ketones and “many” calcium oxalate crystals in my urine. Two liver metrics, alanine transaminase and gamma-glutamyl transferase, were elevated. If he were my doctor, “I would say, ‘Oh, your liver tests are elevated—why is that?’” Hyman told me. “I would ask you a bunch of questions, like ‘Do you drink a lot?’” I don’t—but until recently, I would pop a Tylenol any time I felt even the slightest twinge of a headache setting in, which happened almost every day. Taking too much acetaminophen, Hyman cautioned me, is the most common cause of acute liver failure in the U.S. He appeared pleased that I had gone cold turkey after receiving my results, and I was relieved that I had found out I needed to make a change. (For what it’s worth, this probably wouldn’t have registered on a primary care provider’s annual blood panel, and there’s no way I would have brought up my Tylenol habit unprompted.)
Perhaps most alarmingly, 11 of my 15 heart biomarkers were out of range, suggesting systemic inflammation and an elevated risk of heart events. I wasn’t entirely surprised: High cholesterol runs in my family, and when I was 3, my parents took me to a big-city children’s hospital, where a pediatric cardiologist recommended I start statins. My parents, concerned about my young age, decided not to opt for treatment, and throughout my adult life, I’ve hoped my plant-based diet and exercise routine would shield me from the genetic threat.
Read More: 9 Weird Symptoms Cardiologists Say You Should Never Ignore
Yet the situation was worse than I expected. My total cholesterol, LDL cholesterol, non-HDL cholesterol, HDL cholesterol, apolipoprotein B, and lipoprotein(a) were all out of range. My LDL particle number—a new-to-me term that measures the number of particles carrying LDL cholesterol—turned out to be 2,181, which concerned Hyman. “You want it to be under 1,000,” he told me. All my heart numbers, taken together, indicated to him that I needed follow-up testing, like an AI-enhanced CT coronary scan to check for plaque. I immediately started searching for a cardiologist after doing a deep dive on all the ways a heart attack or stroke might manifest in a relatively young woman.
One of the less-conventional health metrics I learned was my biological age. Inside, I’m 28.5, which is almost 9 years younger than my actual age of 37. This metric indicates the quality and rate of how you’re aging on a genetic, cellular, and molecular level, Hyman says. Faster biological aging—being older than your chronological age—increases the risk of problems like prediabetes, Type 2 diabetes, heart disease, cancer, and hormonal imbalances. While almost every company selling these tests calculates biological age based on a different methodology, Function relies on Phenotypic Age, which is an assessment of biomarkers such as albumin, creatinine, glucose, and mean cell volume.
I asked Hyman if I should be disappointed about my biological age: Wouldn’t it have been better to get a number, say, 15 years younger? “No, no,” he told me—though I soon learned that, while he’s 65, his biological age is 39. (“I’m almost as young as you,” he joked.) He assured me that while you can’t change your calendar age, you can reverse your biological age by, for example, prioritizing a healthy diet, being more active, losing weight, getting enough sleep, and lowering your cholesterol. I’ll have mine retested in six months—and during that time, I hope to get reacquainted with my early 20s, which I thought I had left in the dust.
All of these lab results were accompanied by eight pages of personalized clinician notes; if results are urgent, the company says it calls you immediately. The feedback is dense and actionable: I learned more about what each out-of-range metric meant, and what kind of steps I could take to correct it, like limiting or prioritizing certain foods, taking supplements, and practicing self-care. The calcium oxalate crystals in my urine, for example, suggested a predisposition toward kidney stones, so Function’s clinicians suggested mitigating risk through dietary changes and increased fluid intake. And because my high-sensitivity C-reactive protein—a marker of inflammation—was high, I received a list of dozens of potentially beneficial foods to prioritize (non-starchy vegetables, organic soy), as well as advice on which to limit (refined sugars and dairy).
There were also, of course, abundant suggestions to follow-up with my primary care provider—which put me right back in the doctor-less pickle where I had begun.
The future of health care, or information overload?
My Function Health tests armed me with information—but I wasn’t sure exactly what to do with it. Would primary care doctors and specialists even be interested in reviewing my results? Or would they be annoyed I had taken testing into my own hands (and that they had eight pages of data to wade through)?
Function Health doesn’t yet have an app, which means the easiest way to share results with a doctor is to take screenshots on your phone or print out the relevant sections. Dr. Richard Bruno, regent-at-large with the American College of Preventive Medicine, is used to patients bringing in information for him to review, like Quest blood tests they ordered on their own—but he’s not sure it’s necessary. “I do have patients who [do similar testing], and they come to me with pages-thick labs and want me to interpret it for them,” he says. “Like, ‘Dr. Bruno, what does this mean? It looks like I have kidney function problems.’” That might lead to a conversation about how much value to assign to a slightly out-of-whack sodium level: “Maybe it was because you did a heavy workout this week,” he says. “It’ll probably normalize, because kidneys are very good at normalizing electrolytes.” Sometimes, he’ll run follow-up labs—but notes that pursuing all incidental findings can end up being emotionally and financially taxing for patients.
Read More: Long Waits, Short Appointments, Huge Bills: U.S. Health Care Is Causing Patient Burnout
Still, if you decide to follow through with your own testing, Bruno recommends keeping your provider in the loop—which can also help cut back on Dr. Google-induced anxiety. “Bringing it back to somebody you trust is critical,” he says. “I may chuckle a little if somebody brings me a stack of labs, but I will take the time to help them understand and navigate.”
Dr. Baljash Cheema, an assistant professor of medicine at Northwestern University Feinberg School of Medicine and medical director at the university’s Human Longevity Lab, isn’t convinced Function Health is worth the financial, psychological, and serological investment. He estimates that at least half of the company’s biometrics are related to basic labs he runs all the time. “I don’t know how novel this is,” he says. Plus, he points out that some biomarkers might be too esoteric for all doctors to grasp. “I have to tell you that I don’t know what it means to have your basophil count change from month to month,” he says. “I don’t know if anybody does.” (In case you were wondering: basophils account for about 1% of white blood cells and play a role in the body’s immune response. Mine were normal.) “I’m just not sure that small changes in your potassium or chloride or your lipase or your amylase have true meaning for your health.”
Still, Cheema notes that he agrees with the company’s big-picture goal. “We’re backwards in the way that we approach health care—we wait for disease to show up,” he says. “And I think there is very much a role for preventive screening and getting on top of these things before they cause disease.” Looking forward, he believes doctors will start screening for metrics that give people a better understanding of their longevity, though more work is required to determine exactly what those are, why they matter, whether it’s possible to improve them, and if so, how to do it. “I do think this field is ripe for innovation and really could help people live healthier, longer, better lives,” he says. “But I’m not sure that anything this company is doing right now is doing that.”
A new sense of empowerment
Within the span of a couple weeks, I went from knowing nothing about my health to having more data than I knew I contained. Rabbit holes aside, I felt more invested in my well-being than I had in ages—and motivated to find a care team.
Hyman considers that a victory. “I’m only one guy, so I can only see so many patients,” he says. “I want this to scale up to millions of people.” In the future, he hopes, Function will add even more biomarkers and more depth to its clinician insights. He anticipates steadily increasing demand. “We haven’t done a lot of marketing, and we have 60,000 [paying members],” he says. “So there’s a huge, pent-up need for this.”
He’s in a hurry to start delivering on the largest possible level. Ultimately, he sees Function as a “hub for everyone’s health,” and believes any adult could benefit. “I’m not getting any younger,” he says, before catching his own mistake—because, mind you, his biological age continues to drop. Maybe he is, he concedes. “But I really want to see a shift in this chronic disease epidemic and empower people with their own data, and get this future of medicine here now.”
What's Your Reaction?



























































.jpeg)








































.gif)